New nonwoven microcarriers for cell culture

Scientists at Germany's Hohenstein Institute say that although liposuction has been a standard medical procedure in cosmetic surgery for many years, surgeons are still searching for fat tissue substitutes to provide better treatment for patients with large soft tissue defects. Against this background researchers at the Institute for Hygiene and

24th June 2011
Innovation in Textiles
|
Boennigheim

Scientists at Germany's Hohenstein Institute say that although liposuction has been a standard medical procedure in cosmetic surgery for many years, surgeons are still searching for fat tissue substitutes to provide better treatment for patients with large soft tissue defects.
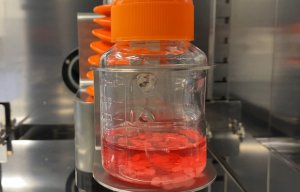
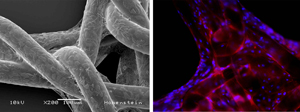
Against this background researchers at the Institute for Hygiene and Biotechnology (IHB) at the Hohenstein Institute have now succeeded in establishing a reasonably sized fat implant under laboratory conditions for the first time. First of all, they successfully differentiated adult stem cells into fat cells while growing them on biodegradable fibres (Fig. 1). Using the same method, they were then able to grow human adult stem cells on three-dimensional implants and differentiated them into fat cells (Fig. 2).
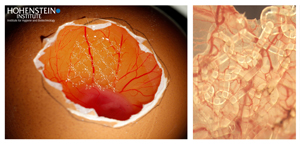
 In reconstructive surgery, replacing soft tissue to treat wounds with large tissue defects is said to represent a great challenge, e.g. in the case of pressure ulcers or large-scale scarring (Fig. 3). Until now, plastic surgeons have been using skin flaps for the reconstruction of soft tissue - a procedure that is said to strongly strain healthy surrounding tissue and therefore the whole patient.
In reconstructive surgery, replacing soft tissue to treat wounds with large tissue defects is said to represent a great challenge, e.g. in the case of pressure ulcers or large-scale scarring (Fig. 3). Until now, plastic surgeons have been using skin flaps for the reconstruction of soft tissue - a procedure that is said to strongly strain healthy surrounding tissue and therefore the whole patient.
"Depending on the size of the tissue defect, tissue expanders are used to stretch the healthy skin and fat tissue for several weeks. It also requires few surgical interventions in order to prepare the wound area and the tissue flaps before transplantation: these processes are associated with many risks for the patient such as hypothermia, cardiovascular problems or wound infections. Currently there is no suitable fat tissue substitute that can be easily transplanted and provides a long-term solution in the treatment of soft tissue defects," the Hohenstein Institute says.
 Textile implants
Textile implantsThe team of scientists led by Prof. Dr. Dirk Höfer, Director of the IHB, is dealing with the question of how textile implants could be complemented with patient's own stem cells so that it can therefore be used more effectively in plastic and reconstructive surgery. The scientists cultivated dense layers of human adult stem cells on fibres, meshes and nonwovens made of biodegradable biopolymers as shown in previous experiments (Fig. 4).
In addition they were able to show that fibre-bound stem cells release growth factors that promote the formation of new blood vessels at the implantation site by using hatched chicken eggs as a vascular model (CAM angiogenesis model). Within a very short time, the researchers say, new blood vessels grew into the biological modified textile implants and formed a functional capillary network (Fig. 5).
 Against this background, the scientists at the IHB continued their work with regard to the development of a fat tissue substitute. Their objective was to establish a biopolymer fibre based soft tissue substitute with enhanced biocompatibility suitable for the treatment of extensive tissue defects. The challenges they face are:
Against this background, the scientists at the IHB continued their work with regard to the development of a fat tissue substitute. Their objective was to establish a biopolymer fibre based soft tissue substitute with enhanced biocompatibility suitable for the treatment of extensive tissue defects. The challenges they face are:
Considering these results, the Hohenstein scientists aimed to grow patient's own stem cells on three dimensional implants made of biopolymers. These adult stem cells could be differentiated into fat cells in order to build a soft tissue substitute without causing inflammatory responses or transplant rejection.
Prof. Dr. Dirk Höfer, (Director of the Institute for Hygiene and Biotechnology at the Hohenstein Institute)
E-mail: [email protected]

Business intelligence for the fibre, textiles and apparel industries: technologies, innovations, markets, investments, trade policy, sourcing, strategy...
Find out more