Solvay helps innovate composite for spinal implants
Researchers at The Hohenstein Institute say they are making progress on the bio tolerance of textile implants by using stem cells to regenerate vascular tissue to allow for optimised integration of textile implants. According to Hohenstein, the capacity of a textile implant to be tolerated by the body, known as bio tolerance, plays an important role in regenerative medicine but the body does not always tolerate textile implants. Even modern implants made of resorbab

13th May 2010
Innovation in Textiles
|
Boennigheim
 Researchers at The Hohenstein Institute say they are making progress on the bio tolerance of textile implants by using stem cells to regenerate vascular tissue to allow for optimised integration of textile implants.
Researchers at The Hohenstein Institute say they are making progress on the bio tolerance of textile implants by using stem cells to regenerate vascular tissue to allow for optimised integration of textile implants.
According to Hohenstein, the capacity of a textile implant to be tolerated by the body, known as bio tolerance, plays an important role in regenerative medicine but the body does not always tolerate textile implants.
Even modern implants made of resorbable biopolymers, such as polylactic acid, are said to break down in the body after a certain period of time and decompose into individual acidic components. They can, the Hohenstein’s scientists say, then cause considerable problems around the implantation site ranging from inflammations to rejection and this is why bio tolerability is a decisive factor in the rapid generation of blood vessels at the implantation site (known as angiogenesis),
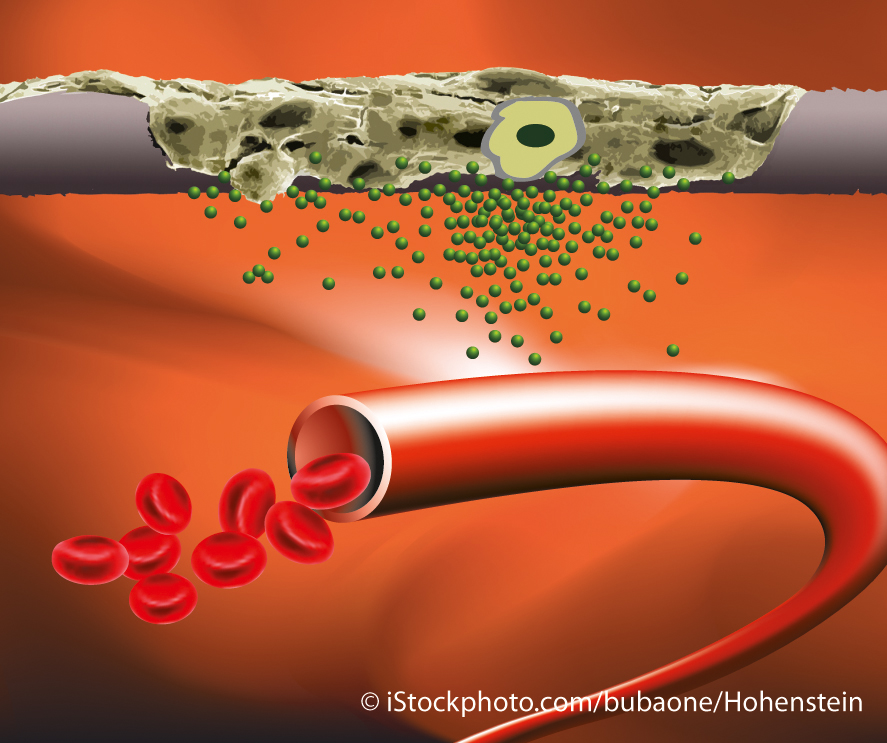
“New capillaries ensure that acidic decomposition products resulting from the breakdown of bioresorbable textile implants can be quickly transported away from the area. At the same time, the new blood supply guarantees that cells involved in building up tissue receive sufficient nutrients and the implant is integrated into the tissue rather than being encapsulated as a foreign body,” the scientists say.
The Institute for Hygiene and Biotechnology (IHB) at Hohenstein has long been carrying out research on how formation of vascular tissue can be stimulated specifically on textile implants. Only recently, a research team made up of doctors and human biologists led by Prof. Dr. Dirk Hoefer showed that specially modified textile fibres are also suited for functioning as a matrix for adult human stem cells on the basis of which new, healthy tissue can be developed.
Now the scientists at Hohenstein say they have successfully carried out a ground-breaking experiment with respect to the tolerability of implants using an animal-free substitute method known as the chorioallantoic membrane assay. Textiles that had been colonised with stem cells were applied onto a chicken egg membrane with a dense network of blood vessels. The dense network of blood vessels of the CAM and its lack of immune competence are said to create create optimal conditions for investigation of a functional circulatory system.
The scientists aim was to have the implant itself release the growth factors required to stimulate the formation of new blood vessels. The stem cells were to assume this function. The researchers first coated the fibres of the textile implants with specific adhesion molecules, then colonised them with adult human stem cells that are known to release growth factors for new blood vessels.
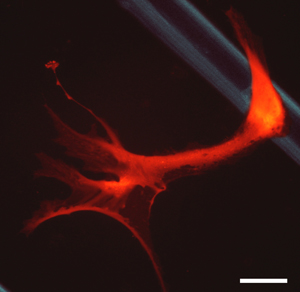
In order to follow precisely the fate of the stem cells, before they were introduced to the implant, the ‘all rounders’ were genetically modified so that they produced a red, fluorescent pigment that allowed the integration of the stem cells in the surrounding tissue to be visually monitored (above right).
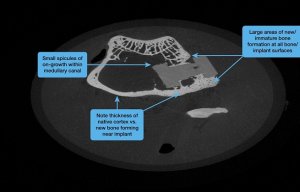
 In several test series conducted in this way, the researchers observed directed vascularisation within the textile implant microscopically and macroscopically (right). New blood vessels grew within the implant and formed a functional capillary network. If the textiles were colonised with connective tissue cells that did not release growth factors, vascularisation did not occur.
In several test series conducted in this way, the researchers observed directed vascularisation within the textile implant microscopically and macroscopically (right). New blood vessels grew within the implant and formed a functional capillary network. If the textiles were colonised with connective tissue cells that did not release growth factors, vascularisation did not occur.
The Institute for Hygiene and Biotechnology's new results may be used in future approaches in regenerative medicine. Implants colonised with a patient's stem cells could serve as biologic textile implants (e.g. hernia mesh implants) that can be integrated into the patient’s body more quickly and without rejection in order to regenerate damaged tissues.
The system applied at Hohenstein is also said to make it possible to gain insights into many other aspects of circulation in textile implants and routinely optimise these implants for medical use. The Hohenstein says this is an important milestone in the further development of textile regenerative medicine and its researchers intend to publish their results in a specialist scientific journal.
Images:
Top
 -Directed formation of blood vessels in a textile implant that has been colonised with stem cells. The dense capillary network is clearly visible. (Scale = 500 μm). Photograph: Hohenstein
-Directed formation of blood vessels in a textile implant that has been colonised with stem cells. The dense capillary network is clearly visible. (Scale = 500 μm). Photograph: Hohenstein
-Negative control: An implant colonised with connective tissue cells in which vascularisation did not take place (scale = 500 μm). Photograph: Hohenstein
-Histological section of the textile implant filled with newly formed capillaries. The capillaries (red) were immune-labelled with the help of specific antibodies (scale = 300μm). Photograph: Hohenstein
Middle
-A PLA-fibre (top right) colonised with adult human stem cells. The cells were genetically modified so that the continually produced the red, fluorescent protein mCherry (scale = 20 μm). Photograph: Hohenstein
Bottom
-Graphic: Textiles colonised with stem cells secrete signalling molecules that stimulate the development of new capillaries from existing blood vessels. Photographs: iStockphoto.com/bubaone/Hohenstein

Business intelligence for the fibre, textiles and apparel industries: technologies, innovations, markets, investments, trade policy, sourcing, strategy...
Find out more